Breast reconstruction after mastectomy
At RAFT, we want to see the same dedication and resolve going into breast reconstruction research that there has been in fighting breast cancer itself.
Help us keep developing Pioneering treatments to restore patients’ quality of life that have suffered physical trauma.
We want to give women worldwide access to better surgery techniques for breast reconstruction after mastectomy; so they can put cancer behind them and focus on the future not their bodies
THE NEED
Breast cancer is THE MOST COMMON CANCER affecting women and one in eight women will develop the disease in their life time.
An estimated 50,000 women are diagnosed with breast cancer each year in the UK, while in the US, more than 230,000 women were diagnosed in 2015 alone.
78% of women will now survive breast cancer for 10 years or more (2011-11 figures for England and Wales).
Treatment includes lumpectomy or mastectomy surgery with adjuvant therapy such as chemotherapy and/or radiation.
Around 40% of breast cancer patients will have a mastectomy. There were 23,200 mastectomies carried out in England in 2011/2012 (NHS). This figure is likely to grow as more women opt for preventive mastectomy following the identification of the BRCA genes.
40% of women suffer from depression post-mastectomy.
CURRENT TREATMENT OPTIONS FOR BREAST RECONSTRUCTION FOLLOWING A MASTECTOMY
Current guidelines recommend that women should be offered the option of breast reconstruction after mastectomy– either immediately or at a later date. The reconstruction techniques available include:
- Artificial implants
- Artificial implant with a tissue transplant from the patient
- Free fat transfer where fat is taken from another part of the body is used to rebuild the breast
- Free flap transfer where tissue including skin, fat and blood vessels are transplanted from another part of the body to reconstruct the breast
However, for various reasons each of these breast reconstruction methods can be unreliable and unsatisfactory. Artificial implants can be rejected; they don’t always look or feel natural and will also need replacing every five to ten years.
Free fat and free flap transfer methods create a more natural look and feel. However, procedures frequently fail when the transferred fat is reabsorbed into the body. The tissue transferred in free flap surgery can also be reabsorbed and tissue rejection is a common risk. Scarring and loss of sensation is also an issue associated with the use of flaps.
As a result patients will require multiple operations which mean long stays in hospital adding to trauma and distress.
A poor surgical outcome is the main reason why fewer than 50% of women who have a mastectomy currently chose to undergo reconstructive surgery.
RESEARCHING BREAST RECONSTRUCTION AFTER MASTECTOMY
Billions of pounds have gone into breast cancer research and treatment, an investment which has radically improved the life expectancy for women with even the most advanced cancers. However, a longer life expectancy means that women who have undergone mastectomy will also live with the physical and mental scars for many years, scars which can easily affect self-esteem, confidence and quality of life.
For most women, breasts are a vital part of identity, yet very little research has gone into improving breast reconstruction after mastectomy.
A NEW APPROACH TO BREAST RECONSTRUCTION AFTER MASTECTOMY
RAFT is working on a novel product which will provide mastectomy patients with a new option for their breast reconstruction, which will not involve the implantation of synthetic material and associated dis-benefits.
The product in development is a 3D ‘scaffold’, built from natural proteins found in breast tissue. It will be used in conjunction with fat and stem cells to help rebuild the breast,. As the breast tissue grows, the implant will be absorbed, leaving behind a natural breast, made with the patient’s own body tissue.
Benefits: Using a scaffold will ensure that the stem cells and fat will stay within the breast reconstruction site rather than dissipating throughout the body. This will help to increase the survival rate and function of the cells after transplant and improve the cosmetic result. Moreover, the biological scaffold is made from proteins which naturally occur in breast tissue and will therefore be metabolised by the body as the new breast tissue is formed.
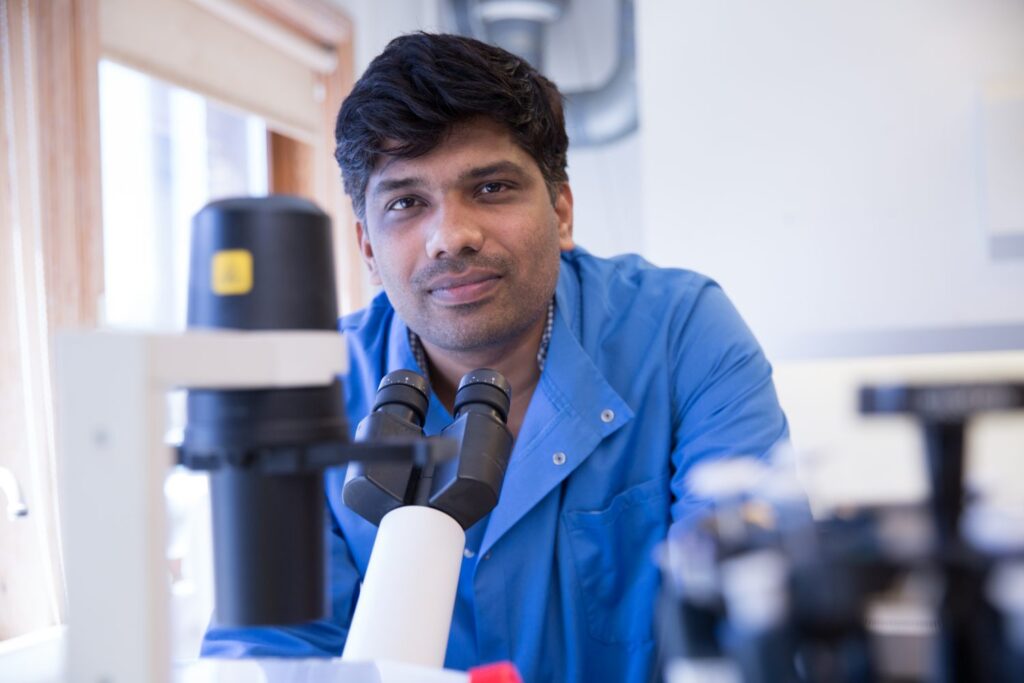
An initial 18 prototypes (with different combinations of natural proteins found in breast tissue) have been subjected to rigorous testing, and a final prototype will be chosen for scaling up into an implant that will be tested in a pre-clinical model (subject to funding). RAFT researcher Dr Prasad Sawadkar (pictured below) is working closely with clinicians to develop an implant that not only improves the lives of patients, but also, more importantly, caters to the surgeons’ needs.
RESEARCH IMPACT
RAFT’s research to improve breast reconstruction surgery will mean that women who have undergone mastectomy:
- Experience less pain and discomfort
- Need fewer operations
- Experience less scarring and numbness
- Have a better, more natural cosmetic result
- Have a reduced risk of tissue rejection
- Experience reduced psychological impact
Ultimately, our research will mean that women can put the black cloud of breast cancer and its aftermath behind them and concentrate on rebuilding their lives.
RAFT RESEARCH SCIENTISTS
- Dr Prasad Sawadkar
- Assoc Prof Elena Garcia
- Mr Oliver Frost
RESEARCH PARTNER AND COLLABORATORS
- The Griffin Institute, Saint Mark’s and Northwick Park Hospitals
- Professor J.C. Knowles, Head of Division of Biomaterials and Tissue Engineering, UCL
- Professor Hae-Won Kim, Director of the Institute of Tissue Regeneration Engineering, Dankook University, Korea
