OUR HISTORY
30 years of medical research
Help us keep developing Pioneering treatments to restore patients’ quality of life that have suffered physical trauma.
RAFT- Our History
WHAT HAVE WE DONE
How we started
RAFT was funded as a medical research charity in 1988 by four plastic surgeons; Roy Sanders, Brian Morgan, Douglas Harrison and Paul Smith, who were dismayed at the lack of successful wound healing treatment options available to patients who had suffered severe burns, such as those injured in oil rig or domestic fires. They were joined by Professor John Scales, the first director of research and Sir Robin Chichester-Clark, the first chairman of the charity.
Where are we today
In 1992 we occupied our own laboratories and office space in the Leopold Muller Building on its own discrete site at Mount Vernon Hospital in Northwood. For many years this was the thriving hub of our research. In 2019 the Trustees recognized that our research, hence our patients, would be better served by moving our laboratories away from a single location that had become progressively less fit for purpose. In 2020 we relocated our key programmes into designated centres of excellence for academic and clinical research, including The Griffin Institute and University College London. In these new homes we continue our research, fully funded and managed by RAFT, but benefitting from state-of-the-art facilities and input from renowned clinical and research collaborators.
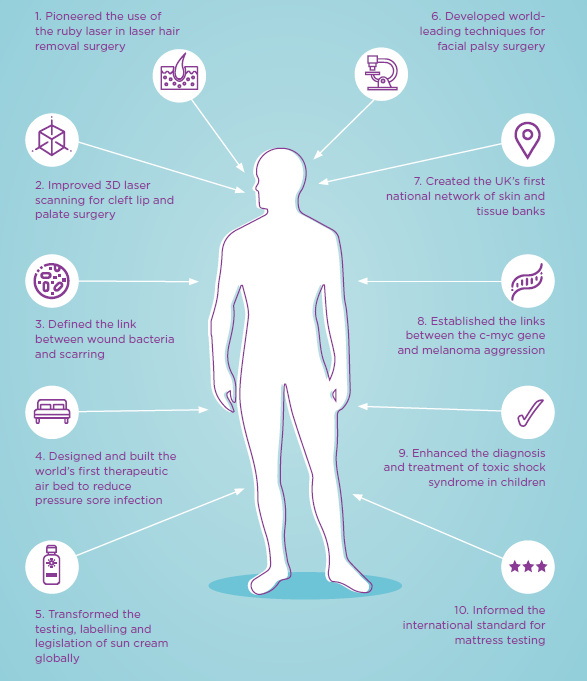
Ten ways RAFT has changed the way we think
For 30 years, scientists at RAFT have developed novel and innovative approaches to problem solving, using science and imagination to change lives.
- Built the world’s first floating bed, supporting patients in the air to treat those with burn and pressure sores
- Used plaster casts of celebrity bottoms to develop the world’s first mattress dummy
- conducted the world’s first trials of insulin as an anti-scarring agent
- discovered a new blood vessel in the human body
- investigated the use of green tea, honey, and sugar for wound healing
- scientifically proved that caffeine and microsurgery dont mix
- pioneered the use of a ruby laser to remove hair for non-cosmetic procedures
- identified the optimum way to apply sun cream to maximise protection
- established the potential for the c-Myc gene as a predictor for cancer
- created new methods for attaching leeches to surgical wounds
Inspiration to Innovation
How a Hovercraft changed Burns Treatment Globally
The path which ultimately led to RAFT began when Mount Vernon Hospital in Northwood, England, became a plastic surgery and jaw injury centre in 1953.
At this time, many burns patients died from sepsis (whole body inflammation) caused by infection. Standard hospital treatment was to leave the burn exposed to open air to dry the injury. However, when extensive burns covered most or all of the patients’ body, the part of the wound touching the bedding remained wet.
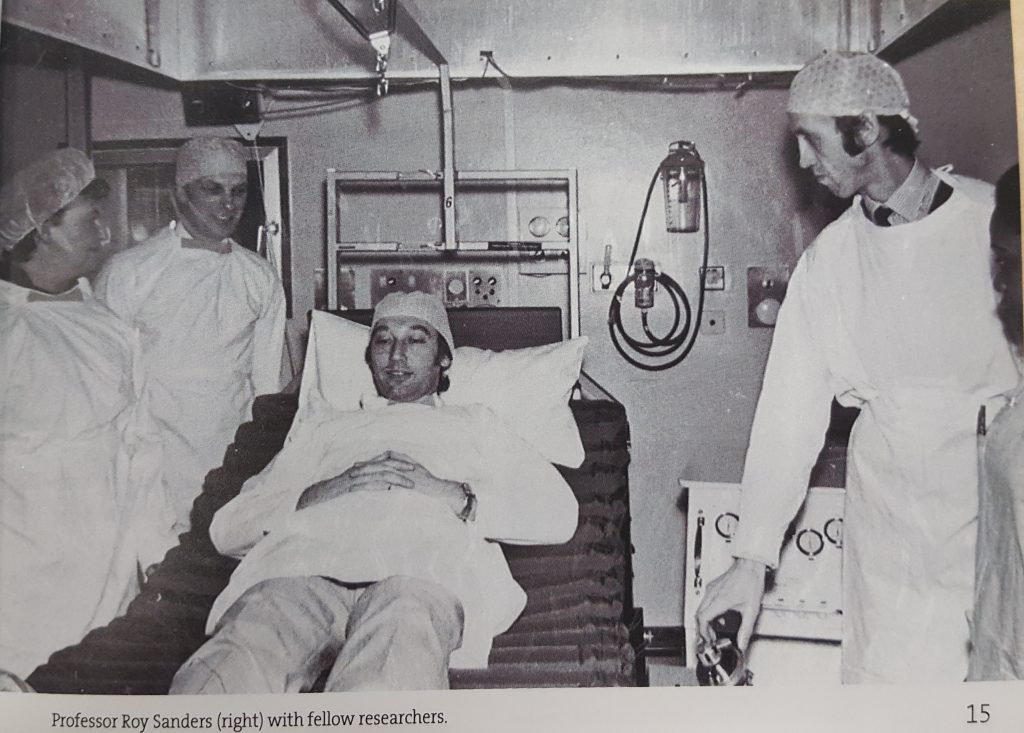
Clinicians at Mount Vernon pioneered raising the temperature of the room to create a ‘mini-desert’ to prevent heat loss, a common problem amongst burns patients, and to speed up the drying of the wound; but that didn’t help where the wound touched the bedding. And that’s where Professor John Scales came in. A biomedical engineer, he took inspiration from a hovercraft and developed the first prototype bed that would allow a patient to ‘float’ on air. Of course, such an innovation wouldn’t just benefit burns patients but also those with other injuries or those at risk of developing pressure sores.
This pioneering work at Mount Vernon hospital not only led to the development of air mattress technology which is now used to help patients globally- it was the beginnings of a Research Institute at Mount Vernon which later became known as RAFT.
Technology to create Medical Advancement
From the start, RAFT has always embraced new technology, an continues to do so today.
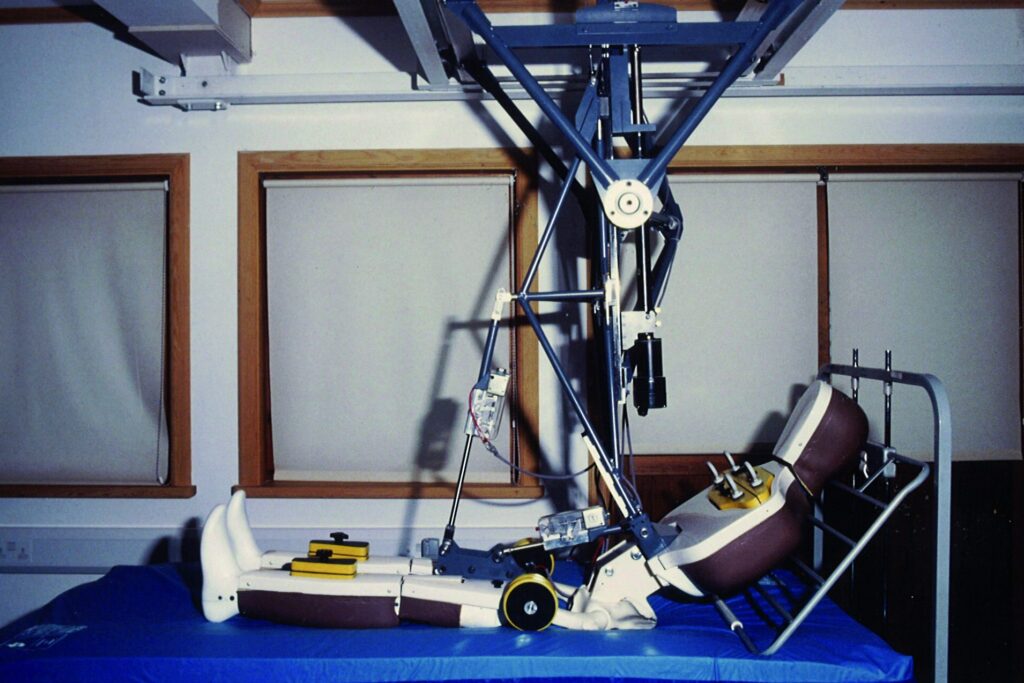
Professor Scales’ work on patient support systems continued during his tenure at RAFT as Director of Research. He recognised that no method existed for testing how well mattresses distributed patient pressure. Even distribution of such pressure is crucial to minimise the risk of pressure sores developing in patients, so Professor Scales devised the idea of a creating a dummy patient for mattress testing.
It was estimated that up to 70% of pressure sores developed on the bottom, so having the right shape on that part of the dummy was crucial. After initially trying to plaster cast people’s buttocks, the research team at RAFT turned to new technology; laser scanning, to create an accurate mould. ‘Gladys’ (pictured, right), as the dummy patient became known, was later born and the rest as they say is history!
SmartMatrix®
TURNING RESEARCH INTO A COMMERCIAL PRODUCT
This is work in progress and is potentially one of the most important developments in the charity’s 30-year history.
The RAFT research team developed a dermal scaffold which works by encouraging the proliferation of skin cells and the growth of new blood vessels, mimicking the natural process of healing in the body. This scaffold provides a treatment solution for certain wounds which the body has difficulty healing; for example, those created by the surgical removal of cancerous tissue. Such wounds are routinely treated with the use of skin grafts. SmartMatrix ® negates the need for a skin graft and will therefore bring benefits to the patent, clinician and health services.
Clinical trials started in 2014 and it is likely to take 10 years to obtain the relevant regulatory approvals before the product can be used by the surgeons.
Alongside the scientific research we established and spun off a separate company, utilising the Enterprise Investment scheme attracting private investors to fund the development of the commercial product . The company is totally independent of RAFT, although we retain the royalties that could translate into future income for the charity.
We are firm in our commitment that, at RAFT, patients’ needs always come first, but we will explore further opportunities for commercialization of our research if this means quicker and broader access for patients, as well as wider sources of funding for further research.

More on the work that RAFT has done to change front line healthcare can be found here: OUR IMPACT.
Read about current RESEARCH PROJECTS here.